Nursing group issues 7 standards on safe staffing
Telehealth Nutrition Program Proves Effective in Fighting Food Insecurity
New codes from the AMA could mean more RPM reimbursement by 2025
The Future of Human Health May Require Unlocking Access to Our Health Data
Why doctors should embrace uncertainty for better patient outcomes
In a single session, we explored shifting perspectives, fostering internal validation, and practicing gratitude and breathwork. The doctor declared it life-changing, prompting reflections on the impact of certainty in healthcare and the potential for broader perspectives to enhance patient care and professional fulfillment.
Read on kevinmd.com
Why Healthcare Software Testing Services Are Important

The healthcare industry is rapidly growing by adopting the latest technological trends. Based on Precedence research – professionals, healthcare companies, and patients demand applications of the highest standards. Therefore, a stringent testing process is necessary for this programming product. The quality of medical products and services offered to users must be impeccable. Let’s delve into the critical elements that help to achieve optimal healthcare software.
Healthcare Industry Features
The healthcare sector heavily depends on specialized platforms, including electronic health record (EHR) systems, telemedicine platforms, and health information exchange (HIE) networks. Ensuring adherence to industry-specific standards, such as DICOM (Digital Imaging and Communications in Medicine), is crucial for seamlessly integrating and managing data from diverse sources. Moreover, the practical functionality of healthcare technology necessitates seamless integration with various applications and microservices, encompassing software for medical devices and payment processing. Several big healthcare companies have embraced applications to enhance operations, improve patient care, and streamline various healthcare processes. Here are a few examples:
Epic Systems Corporation: Epic Systems is renowned for its electronic health record (EHR) system, Epic. Large healthcare organizations have widely adopted the Epic EHR system to manage patient records, appointments, billing, and more.
Cerner Corporation: Cerner offers a range of healthcare information technologies, including its electronic health record platform. Healthcare providers use Cerner applications to digitize and optimize clinical, financial, and operational processes.
McKesson Corporation: McKesson provides healthcare management solutions, and its applications are utilized for pharmaceutical distribution, health information technologies, and medical supplies management. Their applications contribute to the efficient functioning of healthcare systems.
IBM Watson Health: IBM Watson Health utilizes artificial intelligence (AI) applications for healthcare analytics, drug discovery, and personalized medicine. Their applications leverage data to provide insights for both healthcare providers and researchers.
These examples demonstrate how healthcare companies use applications to enhance patient care, improve operational efficiency, and stay ahead in the healthcare industry.
The Key Aspects and Objectives of Healthcare Software Testing Services
Healthcare software must adhere to high-quality and performance standards to ensure it functions reliably and efficiently. Healthcare software testing services help identify and address different types of software issues.
Safety and Adherence: Safety and adherence are paramount, given the sensitive nature of healthcare data and the regulatory environment. Healthcare software testing helps to ensure that applications comply with industry regulations, such as HIPAA, and adhere to safety standards to protect patient information and ensure the well-being of patients.
Accuracy and Cross-Dependency: Accuracy is crucial in healthcare software, as errors can have significant consequences. Healthcare testing services help to verify the accuracy of data processing and ensure that the software integrates seamlessly with other entities, promoting interoperability and reducing the risk of errors caused by cross-dependency.
Reliability and Efficiency: Healthcare software needs to be reliable and efficient to support the timely and accurate delivery of patient care. Testing helps identify and address system reliability, responsiveness, and overall efficiency issues, contributing to a positive user experience for healthcare professionals and patients.
User-Friendliness: The ease of use of healthcare software is a critical factor in its adoption and effectiveness. Testing, including usability one, helps ensure the software is user-friendly, improving efficiency for healthcare professionals and making it easier for patients to interact with the system.
Legal and Regulatory Compliance: Healthcare organizations must adhere to various laws and regulations. Testing services verify that the software aligns with federal, state, and local laws and third-party payer obligations. This is crucial for avoiding legal issues and maintaining the trust of stakeholders.
The Importance of Healthcare Software Testing
In healthcare software, testing plays a pivotal role in helping to ensure optimal outcomes. Here’s why:
Patient Safety
Specific healthcare software is often used in critical situations, such as patient diagnosis, treatment planning, and monitoring. Errors or bugs in the software can lead to incorrect diagnoses or treatments, jeopardizing patient safety. Rigorous testing helps identify and rectify such issues, ensuring that the software functions accurately and reliably.
Regulatory Compliance
The healthcare industry is carefully regulated to ensure patient information privacy and high-quality healthcare services. Healthcare software must comply with various governing requirements, such as the HIPAA in the United States. Testing helps ensure that software meets these controlling standards.
Data Security
Security breaches can have serious consequences, such as identity theft or unauthorized access to confidential medical information. Identifying and addressing security vulnerabilities and protecting patient data from cyber threats and unauthorized access is crucial.
Usability and User Experience
Healthcare professionals use various software applications daily. Usability testing helps ensure that these applications are user-friendly and intuitive. A well-designed and easy-to-use software interface can help to improve efficiency and enhance the overall user experience for healthcare professionals.
Cost-Effectiveness
Identifying and fixing software issues early in development is more cost-effective than addressing them after the product has been deployed. Comprehensive testing helps catch and report bugs, reducing the risk of post-deployment issues that may lead to costly emergency fixes or system downtimes.
Continuous Improvement
Healthcare software continually evolves to adapt to new technologies and meet changing medical needs. Regular testing is essential for identifying areas of improvement, ensuring that software stays up-to-date, and incorporating new features or updates without compromising quality.
Services Provided by Luxe Quality
Luxe Quality specializes in providing healthcare testing services, helping ensure our clients’ highest quality standards.
Web App Testing
Web App Testing is a critical phase in the software development life cycle that focuses on verifying web applications’ functionality, performance, and security. This process ensures that web applications work as intended, providing a positive user experience across browsers and devices.
Mobile App Testing
Mobile App Testing helps to ensure mobile applications’ seamless functionality, usability, and security across various devices and platforms. This process involves rigorous testing of features, regression, performance, compatibility testing, and user experience to deliver a high-quality and reliable mobile app.
Security Testing
Security testing aims to identify and address vulnerabilities and weaknesses in a system to safeguard digital assets and sensitive information against security threats and unauthorized access. This testing process involves evaluating the application or system for potential security risks, such as data breaches, unauthorized access, and cyber-attacks.
Compliance Testing
Compliance testing helps to ensure that healthcare systems comply with regulations and standards, like HIPAA in the USA and GDPR in Europe, to maintain patient confidentiality and data privacy.
Data Integrity Testing
Ensuring the accuracy and consistency of data processed in healthcare systems is crucial for maintaining the integrity of patient records and medical information.
Recovery Testing
It assesses how an application behaves after an unexpected external impact, like a power outage, internet connectivity loss, or device unplugging. Testing an application’s ability to recover gracefully from disruptions is essential to minimize data loss and maintain operational continuity during unforeseen events.
Usability Testing
Patients’ unique requirements and viewpoints must be understood and incorporated to create a user-friendly application.
Accessibility Testing
Accessibility testing is essential to ensure that a product meets the needs of users with disabilities, promoting inclusivity and enabling equitable access, which is particularly critical in healthcare applications.
Performance Testing
Performance testing is vital to assess an application’s responsiveness and stability, especially in scenarios where numerous clients may simultaneously use the app, such as scheduling appointments. It helps to guarantee a seamless and efficient user experience.
Conclusion
Effective software testing in the healthcare sector is vital for optimal application performance. It covers compliance, security, UI/UX enhancements, medical device testing, and interoperability checks. Healthcare testing services help to guarantee accuracy, efficiency, and reliability in healthcare systems. As technology drives healthcare innovation, software testing ensures precision and improves patient outcomes.
Getting into Medical Schools: Tips and Recommendations for Students in 2024
Aside from being a highly renowned and profitable career across multiple markets, medicine is what will let you combine your desire to assist people in their needs and your passion for research. If you want to become a successful doctor, though, your first steps in the field are of great importance. No matter how intense the competition is for prospective students, knowing potential pitfalls and how to avoid them will surely make your path more streamlined and efficient.
Keep on reading this guide to see what preparations will come in handy before and during your first year of studies in a chosen medical school.
Junior- and Senior-Year Preparations for Medical Schools
Typically, the start of the application process for junior students to enter medical establishments starts in the last month of spring. One thing future students always disregard is that they don’t have to rush their preparations. If you aren’t ready for the current season, it is better to build up a better portfolio and write my essay for proper admission rather than lose your chance for a better educational environment.
Focus on your curriculum to get better grades and prepare for exams — don’t let the worries about your future Bachelor’s degree ruin your academic performance. It won’t be extra to glance at what GPAs successful candidates have to have to be accepted as medical school students. Here is a little recommendation: there is no need to focus only on last year’s data.
August through December
Focus on pre-med courses and other classes that will assist in your future application. If you haven’t done this already, it is also the right moment to consult with a professional advisor about your next steps in the field.
January to March
It is the right moment to take your time and take care of your extracurricular and academic performance in more detail. You will need to showcase your exposure to medical science, so publications or hands-on experiences will come in handy for sure. For example, you can additionally apply for a summer camp or internship to increase the likelihood of being accepted as a student in the medical school of your dreams. Of course, don’t forget about your MCAT scores.
April and May Applications
In general, students will require three letters of recommendation. Their quality and variety will boost your chances during the initial and secondary screening process. Your task is to ensure you get assistance from a few types of recommenders with different backgrounds. For instance, you can ask your internship supervisor and professor for corresponding help. This will help you showcase your soft and hard skills from different angles.
June and August Applications
Your primary applications won’t be complete without letters of recommendation, MCAT scores, and other details about your extracurricular achievements and academic accomplishments. If you catch the eye of the desired school, its application admission board will provide you with a secondary application. That’s when you define your real chance to enter the target school and stand out among other candidates.
Applications for Seniors from Fall through Spring
Patience is key. Given that such admissions take place regularly, a lot of data will be analyzed during the process — if you aren’t enrolled during the initial stage, it doesn’t mean you won’t succeed in the next one. The rule of thumb is to proceed with as many applications as you need in a timely manner. Those who don’t have a certain idea of schools to apply for by April 30th, especially in the AMCAS frames, won’t be able to accept more offers later on.
Choosing the Best Application Service
There are several application services in the United States to be aware of before concluding your preparations. Although American Medical College Application Service is the most dominant in the market, others don’t fall behind drastically. If you rely on AMCAS, you will benefit from your decision to pursue most allopathic medical programs. The fees depend on how many schools that are regulated by the service you apply for — $160 for your first application and around $40 more for each next submission. Its deadlines are from May 2nd to August 1st for early decision programs.
Here are a few more big organizations to consider:
- AACOMAS — it will be the right choice for people interested in studies under the roof of osteopathic programs. While the application process starts on May 1st, each school decides individually what deadlines their students have to adhere to. It is also on the more expensive side — $40 for additional applications and $195 as the initial payment.
- TMDSAS — compared to other offers, it is the most affordable one — a one-time fee of $160 for all the applications you are going to make. The deadline for submitting your submission to schools that participate in the Texas Medical & Dental Schools Application Service is September 29th.
To consider what medical schools to include in your application tactics, check their offers from multiple perspectives:
- what special interests and strengths they offer;
- grading system peculiarities;
- finances and what grants are applicable;
- location;
- competition level by seeing your position versus other students in the MCAT and GPA score ranking.
Wrapping It Up
Getting ready to join the target medical educational establishment’s community as a student isn’t a fast process — it can easily take two years of effort and research. At the end of the day, coping with the procedure in bite-sized parts, as this guide suggests, will drastically simplify your preparations and reduce the hassle and risk of mistakes. Once you’ve chosen a selection of schools that cater to your career and research interests, consider their requirements. This strategy will help you make your approach personalized yet versatile and data-driven.
Exploring Cosmetic Dentistry: Discover Your Path to a Brighter, Whiter Dental Aesthetic
In today’s image-conscious world, having a bright, beautiful smile has become a top priority for many individuals. A radiant, well-aligned set of teeth can boost your confidence and make a lasting impression in both personal and professional settings. Fortunately, cosmetic dentistry offers a range of innovative solutions to help you achieve the smile of your dreams. Wondering what solutions?
Relax! In this article, you will explore the various techniques and treatments available in cosmetic dentistry that can transform your dental health and aesthetics. From teeth whitening to advanced orthodontic solutions, you’ll discover each procedure and which might best fit your specific needs.
So keep reading!
Understanding Cosmetic Dentistry
Cosmetic dentistry includes several procedures, each tailored to meet specific aesthetic goals. These treatments improve your appearance and can contribute to functional dental improvements, enhancing your oral health and your smile.
Teeth Whitening: This is perhaps the most popular cosmetic dental procedure. Over time, teeth can become stained from food, drinks, smoking, or poor oral hygiene. Professional teeth whitening offers a quick and effective solution to brighten your smile significantly, far surpassing the results of home whitening kits.
Dental Veneers: Veneers are thin, personalized shells crafted from porcelain or composite material designed to cover the front surface of teeth. They are an excellent choice for correcting imperfections such as severe discoloration, chips, or misshapen teeth.
Dental Bonding: In this procedure, a durable plastic material is applied to the teeth and then hardened with a special light, ultimately bonding the material to the tooth. Bonding is used to repair decayed, chipped, cracked, or misshapen teeth; it’s also a good cosmetic alternative to amalgam fillings.
Dental Implants: For those missing teeth, implants provide a long-term solution that can improve your smile aesthetically and functionally. A dental implant involves a titanium post being surgically inserted into the jawbone, which supports a crown, resembling and functioning like a natural tooth.
Orthodontics: While traditionally not categorized strictly under cosmetic dentistry, today’s orthodontic treatments often serve dual purposes—functional and aesthetic. Treatments like Invisalign offer a less noticeable, more aesthetic alternative to traditional metal braces, and they are chosen by many adults.
But remember, when it comes to cosmetic dentistry, choosing professionals with experience is crucial. Why? One of the top cosmetic dentist, Dr. Samadian, says that you can achieve the ideal smile that you have always dreamed of with a professional. They use advanced techniques and technology to ensure the highest quality of care and the best possible outcomes for their patients. Additionally, experienced professionals have a proven track record of success and can offer valuable guidance and advice throughout the cosmetic dental journey.
So, before embarking on any cosmetic dental procedure:
- Research reputable dental professionals with experience in cosmetic dentistry.
- Schedule a consultation to discuss your goals and concerns with the dentist.
- Ask about the specific procedures available and their potential outcomes.
- Inquire about the risks and benefits associated with each treatment option.
- Review the cost of the procedure and consider your budget and financing options.
Benefits of Cosmetic Dentistry
The benefits of cosmetic dentistry extend beyond just aesthetics. Read below to know;
Confidence Boost: With a more radiant smile, you’ll feel more comfortable and confident in social situations, whether it’s posing for photos or engaging in conversations with others. The newfound confidence in your smile can positively impact various aspects of your life, from personal relationships to professional opportunities.
Improved Oral Health: Many cosmetic treatments also contribute to better oral health by addressing underlying dental issues. For example, fixing misaligned teeth can improve oral hygiene, reducing the risk of gum disease and tooth decay.
Enhanced Appearance: These procedures can transform your smile, correcting imperfections such as stains, chips, or misalignments. With treatments like teeth whitening, veneers, or orthodontics, you can achieve a brighter, straighter smile that boosts your confidence and self-esteem.
Functional Benefits: Beyond aesthetics, cosmetic dentistry can also improve the functionality of your teeth. Treatments like dental implants or veneers not only enhance appearance but also restore proper bite alignment and chewing ability.
Long-Term Investment: While there’s an initial cost, cosmetic dentistry procedures can last for years with proper care, making them a worthwhile investment in your smile and overall well-being.
Conclusion
Now you know! Cosmetic dentistry isn’t just about vanity – it’s about creating a smile you love that can benefit your confidence, oral health, and overall well-being. So, why wait? Take charge of your smile’s future. Schedule a consultation with a qualified cosmetic dentist today and discuss the possibilities. With advanced techniques and experienced professionals, your dream smile is closer than ever!
Healthcare Workforce Trends: Staffing Ratios and Job Satisfaction
In the world of healthcare, both professionals and patients are on the brink of a revolution, driven by rapid technological advancements and groundbreaking innovations.
These changes are not only reshaping the way care is delivered but are also significantly altering the landscape of employment within the industry
As new technologies emerge, they bring with them a burgeoning demand for a diverse range of skills and expertise, creating both challenges and opportunities for healthcare facilities and workers alike.
This evolving scenario calls for a deeper understanding of how staffing trends and job satisfaction are intertwined with the future of healthcare.
The Crucial Role of Staffing Ratios
Staffing ratios—the number of healthcare providers to patients—remain a fundamental metric in healthcare management.
These ratios are critical because they directly impact the quality of patient care and the work environment for staff. Optimal staffing ensures that patients receive the attention they require for their health needs, which in turn facilitates better recovery outcomes.
In many healthcare settings, especially those experiencing staffing shortages, the workload can become overwhelming, leading to increased stress and burnout among healthcare workers. This not only affects their health and job satisfaction but also the quality of care provided to patients.
For instance, research indicates that hospitals with favorable nurse-to-patient ratios see significantly lower readmission rates and better patient outcomes compared to those with less favorable staffing.
A study from Science Direct found that increasing the nurse staffing ratio by just one patient per nurse could reduce hospital readmissions by up to 5%.
Trends Influencing Staffing Ratios
Several trends currently influence staffing ratios in healthcare. Such as:
Aging Population
The growing number of elderly individuals is escalating the demand for healthcare services. This demographic shift requires more hands on deck, particularly in specialties dealing with chronic and age-related conditions.
Technological Advancements
While technology promises greater efficiency, it also demands new skills and continuous learning from healthcare professionals.
Technologies such as telemedicine, robotic surgery, and AI-driven diagnostics require specialized training, thus impacting staffing as facilities must consider both numbers and capabilities.
Regulatory Requirements
Different regions have responded to staffing challenges by implementing regulatory measures. For example, certain U.S. states have enacted laws specifying minimum nurse-to-patient ratios in an effort to standardize care quality across facilities.
Job Satisfaction Among Healthcare Workers
Job satisfaction in the healthcare sector is closely linked to staffing levels.
Adequate staffing not only reduces the pressure on existing staff but also improves their job satisfaction by creating a less stressful and more supportive working environment.
Research by Butterworth et al. (1999) highlighted the significant stress levels British nurses face, with occupational stress on the rise.
It was reported that 40% of hospital nurses experienced burnout, and one in five considered leaving their jobs within the following year. This is because they endure considerable stress due to long working hours, a wide range of tasks, and complex relationships with patients, their families, and co-workers.
Addressing Challenges through Strategic Approaches
Innovative Recruitment and Retention Strategies
Attracting and retaining skilled healthcare professionals is more critical than ever. Innovative strategies such as offering competitive salaries, flexible work schedules, and opportunities for professional development are vital.
Additionally, creating a supportive work environment that values each team member’s contribution can improve retention rates.
Leveraging Technology to Optimize Workforce Management
Healthcare facilities can use advanced scheduling software to optimize staff allocation based on patient acuity and predicted admission rates. These tools can help manage workload distribution more effectively, ensuring that no single team or individual is overwhelmed.
Enhancing Training and Education
Continued education and training programs are essential for keeping staff at the forefront of the latest medical advancements. Investing in education not only equips healthcare professionals with the necessary skills but also contributes to job satisfaction as they feel more competent and valued. Incorporating provider credentialing services into these training programs ensures that all credentials are up to date, further enhancing staff competency and compliance.
Fostering a Positive Work Culture
A positive work environment that promotes team collaboration, respects personal time, and recognizes hard work is crucial for job satisfaction. Regular feedback sessions and team-building activities can enhance the work culture significantly.
Embracing Outsourcing
Outsourcing non-core activities such as revenue cycle management to a medical billing company significantly alleviates the workload on healthcare staff.
By delegating tasks such as administrative duties, billing, and even certain clinical support services to external providers, facilities can allow healthcare professionals to focus more on patient care.
This approach not only streamlines operations but also can enhance job satisfaction by reducing the stress and burnout associated with juggling multiple responsibilities.
Conclusion
As the healthcare industry continues to evolve under the influence of demographic shifts, technological advancements, and regulatory changes, understanding and adapting to the trends in staffing ratios and job satisfaction becomes imperative.
Healthcare providers and facility owners must stay informed and proactive in addressing these trends to ensure that they not only meet the standards of care but also maintain a satisfied and motivated workforce.
Through strategic planning and thoughtful leadership, the challenges presented by these trends can be transformed into opportunities for growth and improvement.
How Dental IT Practices are Shaping Modern Dentistry
While advancements in tech have significantly transformed the medical industry for decades, dentistry has certainly taken its time to get up to speed and adopt IT, digital tools, and processes that could potentially revolutionize the sector.

A shallow focus of a female dental technician designing a new dental prosthesis in a clinic
The good news is that as technology becomes more streamlined, more accessible, and more affordable, the benefits are beginning to outweigh the cons for dental practitioners when delivering quality care to their clients. Coast Dental is one of the leading surgeries employing top tech services in 2024.
A closer look at dental IT
Advancements in artificial intelligence, digital tools and software, and even aspects like 3D printing are quickly becoming go-to solutions in dentistry. With so many advantages linked to each of these, let’s take a closer look at what dentists can expect:
AI in dentistry
Artificial intelligence has the unique ability to adapt and learn as it is used, and its applications are wide and varied across the dental industry. Not only can it assist in elevating patient care, but it can also in streamline a host of front-end, back-end, and B2B operations.
It is not yet widely used in robotics for physical patient care, but it is becoming more prevalent for imaging and diagnosis, analysis and predictive analysis, treatment planning, and administrative support. There’s also a growing interest in the potential advantages of augmented and virtual reality-driven scenarios.
The most attractive benefits of AI in dentistry include faster diagnosis and earlier treatment of patient conditions through imaging and the accessibility and shareability of information between a host of practitioners, dentist offices, and healthcare spaces.
Digital tools and software in dental practices
A host of digital dentistry tools and software can be leveraged to streamline data analysis and boost predictive treatment protocols. One of the biggest hurdles in medical fields and dentistry is the fact that historical data can be extremely difficult to examine, share, and derive insights from. This is largely due to how medical records are kept. Digital tools and software can be installed and use AI algorithms to crunch numbers at lightning speeds and create personalized treatment plans and preventative care strategies. On the other hand, software can be used to improve record taking for the future and connect multiple and even multinational individuals to patient data.
3D printing in dentistry
3D printing is one of the only technological advancements being applied to dentistry that is supported by hardware. Data can be taken from imaging and AI programs and transmitted to a 3D printing device that will be able to produce custom solutions for everything from prosthodontics and dental, craniomaxillofacial, and orthopaedic implants to the production of drill guide implant frameworks and a host of components for both dentistry and maxillofacial surgery.
Are dental IT practices better than traditional approaches?
While there are many arguments both for and against the use of AI in many sectors, dentistry can certainly benefit from implementing specific IT practices. Traditional approaches may be tried and tested, but there have been challenges in recent years that technology has the ability to address for the benefit of patient care and collaboration for the wider industry.
8 Mindblowing Examples Of Technology Innovation In Healthcare
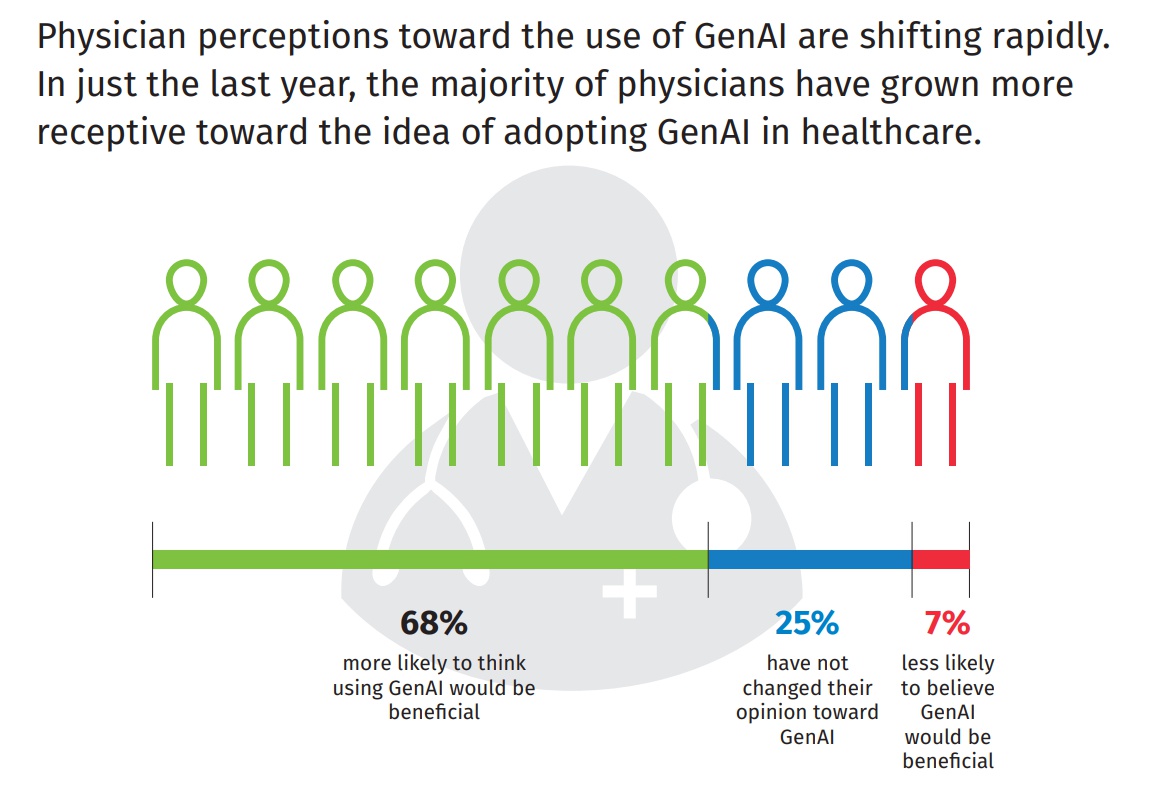
US Physicians Embracing Generative AI for Patient Care, But Transparency is Key
Healthcare App Design: Boosting User Experience and Effectiveness
In healthcare, a well-designed healthcare app can be a lifesaver – literally. If done right, it’s a powerful tool that can transform how care is delivered and how patients manage their health.
Healthcare apps should make life easier for users. That means that a truly successful application has to be built with how people actually use it in mind.
Peter Morville’s UX Honeycomb is a great way to break down UX design’s components:
- Usefulness. Does this actually help someone? Does it make managing their health simpler?
- Usability. Can people figure it out, or will opening it cause a headache?
- Desirability. Does it look and feel good enough that people want to use it?
- Findability. Can people easily find that old test result or setting?
- Accessibility. Everyone should be able to use the best tools for their health. Does it work for people with disabilities?
- Credibility. Health info is serious. Does the company and app feel trustworthy and secure?
- Is it worth the effort, or will it sit unused on their phone?
These are the kinds of questions that make for amazing healthcare apps. Every top digital product design company understands that it’s not just about the features — it’s about the whole experience fitting into people’s lives.
Challenges in Healthcare App Design
Healthcare apps have the potential to make a real difference in people’s lives, but let’s be honest, designing them isn’t exactly a walk in the park.
Here’s why:
- The complexity of healthcare data. Healthcare app design needs to make that dense health data feel understandable, even actionable. But how to achieve this is something that a designer should have in mind.
- Privacy and security concerns. In healthcare, one security slip-up can have serious consequences. Balancing top-notch protection with a user-friendly app is a major design task. Designers must adhere to strict regulatory standards, such as HIPAA in the United States or the DPA 2018 in the United Kingdom. Privacy policies should be made easy to understand.
- Integration with existing systems. Getting hospital and clinic systems to communicate with an app is no easy feat, even for an experienced designer. Your app’s ability to function with a hospital or clinic’s electronic health record (EHR) system is crucial.
- Diverse user base. Picture the range of people using a healthcare app – from young people who live on their phones to seniors who might be less tech-savvy, and even rushed doctors needing info on the fly. Trying to design something that works for everyone is a tall order.
Approaches for Overcoming Challenges in Healthcare App Design
As noted earlier, healthcare app designs have their own unique set of challenges, but with the right approaches, they can be tackled:
- A/B Testing. According to Harvard Business School, A/B testing increases performance in various areas. With A/B testing, you show two slightly different versions of a feature, content, or design to different groups of users to know which one they’d prefer. This data-driven approach takes the guesswork out of design.
- Heuristic Evaluation. Sometimes, you need fresh eyes. Usability experts conduct heuristic evaluations — a design checkup according to established principles of heuristics to help spot potential hiccups in app design.
- Card Sorting. Card sorting helps you find out how your app should be organised. You give users “cards” representing different app features, and they group them in ways that make sense to them.
4 Features That Improve Healthcare App Design
Let’s talk about some specific features that make a real difference in how people use them and how they impact health:
1. Progress Visualisations
Do you know how most people’s eyes glaze over at a spreadsheet of health numbers? Visualisation techniques help present health info in a comprehensible manner.
You can handle visualisation using the following:
- Line graphs. They’re good for tracking trends and can help show how those blood pressure meds are kicking in, or how medication adherence is making a real impact on mood stability.
- Bar Charts. They are perfect for the “before and after” story — pre-treatment lab results vs. now. That side-by-side bar chart can be motivating.
- Area Charts. Ever wonder why sleep quality is so inconsistent? These charts let users visualise those patterns alongside mood, or see how pain levels spike in the afternoon.
2. Biofeedback Integration
When you design an app that has a real-time conversation with the user’s body, you open up a whole new level of engagement and potential for behaviour change.
Through sensors (in wearables or connected devices), a user’s physiological data, like heart rate, breathing patterns, or muscle tension, is fed directly into the app, allowing them to get a more comprehensive picture of their health and risks and act proactively to improve their health.
With gamification, users can engage in healthy lifestyle patterns or behaviours, turning some boring tasks (like treatment plans) into exciting games.
3. Mood-Enhancing Colour Schemes
Our brains are wired to react to colour on a basic level. Colour psychology is a tool you can use to create a positive emotional experience for users.
Check out these healthcare app staples:
- Calmness and Trust. Blues and greens are the ultimate chill pills for our eyes. Perfect for apps where people might be anxious about their health or need to zone in for a meditation session.
- Positivity and Energy. Pops of orange and yellow pump up that “I can do this!” energy in the right context.
- Cleanliness and Sterility. Hospitals use so much white and light grey they project a sense of cleanliness and professionalism.
4. Blockchain-Powered Health Data Security
It’s understandable that blockchain can be a buzzword overload, but it has serious potential to make health data way more secure.
- Blockchain is like a digital record book that can’t be tampered with. Once the data is recorded on a blockchain, it’s impossible to change or delete it without the consensus of other participants of the network.
- Blockchain uses cryptography (hashing and digital signatures) for secure data transfer and access.
- Blockchain is harder to hack compared to traditional centralized systems. This adds to the security of sensitive healthcare data.
Conclusion
Designing a healthcare app that people want to use requires employing various design concepts and trends. A good product needs to fit into someone’s life, help follow treatment plans, make the routine a habit, and highlight potential risks while educating on how to minimise them.
Healthcare apps can be exciting and fun to use if there are visuals, game elements, intuitive navigation, and nice colour palettes. When done right, they can improve lives, build trust, and revolutionise the patient experience.
7 healthcare startups make AI 100
Change Healthcare cyberattack inflicts severe damage on physician practices
AMA survey paints a grim picture of the aftermath of the cyber-attack, with an 36% of respondents reporting the suspension of claim payments.
The American Medical Association (AMA) has disclosed the profound and lasting repercussions of the Change Healthcare cyberattack, illustrating the precarious state of physician practices across the United States. The findings, unveiled in an informal survey report, underscore a landscape fraught with financial turmoil and jeopardized patient care in the wake of the devastating hack.
Conducted from March 26 to April 3, the survey found that 36% of respondents reporting the suspension of claim payments. Furthermore, 32% lamented their inability to submit claims, while 22% found themselves unable to verify eligibility for benefits. Particularly vulnerable to the fallout are practices housing ten physicians or fewer, bearing the brunt of the crisis.
Read on medicaleconomics.com
ChatGPT's potential impact on preventative care and emergency visits
Large language model AI can help with the redistribution of routine tasks to non-physician staff and directly to patients, getting patients to take an active role in their healthcare journey, and enhancing patient engagement and self-management, an expert says.
ChatGPT has been making an impact on enduring healthcare challenges. Many providers and patients are reporting the artificial intelligence helping with preventative care and preventing non-emergent emergency department visits.
Imran Qureshi is chief technology officer at b.well Connected Health, a FHIR-based interoperability platform vendor. He has expertise in AI and a lot of advice to share on the subject of health systems harnessing ChatGPT and other large language model-based technologies.
Read on healthcareitnews.com
Digital Health Apps Graveyard: Why 53% Fail and How to Succeed
Health care organizations collaborate on best practices for value-based care
Mercy saves $30 million in 2023 with AI-powered nursing workforce management tech
Guide for Creating Annotated Biographies in Student Medical Research

Creating annotated bibliographies is an essential skill for student medical researchers. It involves not only listing sources but also providing a summary and critical assessment of each reference. This guide is tailored to help you craft a comprehensive and effective annotated bibliography, which is crucial for supporting your research and understanding the scope of your study within the field of medical research.
What is an Annotated Bibliography?
An annotated bibliography is a detailed list of citations to books, articles, and documents. Each citation is followed by a brief (usually about 150 words) descriptive and evaluative paragraph, known as the annotation. The purpose of the annotation is to inform the reader of the relevance, accuracy, and quality of the sources cited.
What is Student Medical Research?
Student medical research refers to scholarly activities undertaken by students in the medical field to expand knowledge, test hypotheses, and explore innovative solutions to health-related questions. This type of research can encompass a variety of methodologies, including experimental, observational, and theoretical studies. Students might investigate drug efficacy, explore disease mechanisms, improve surgical techniques, or evaluate public health interventions.
The purpose is not only to contribute to medical science but also to enhance the students’ learning experience through practical engagement with their field of study. By participating in research, medical students develop critical thinking, problem-solving skills, and a deeper understanding of evidence-based medicine.
Why is it Important in Student Medical Research?
In the context of medical research, an annotated bibliography serves multiple purposes:
- Enhances Research Skills: It helps students learn to find, analyze, and digest relevant literature efficiently.
- Promotes Critical Thinking: Evaluating sources encourages critical thinking about the content and its application to your specific research area.
- Provides a Literature Review: It offers a snapshot of the current knowledge and debates on a particular topic.
- Supports Research Proposals: It is often used to justify the need for research and to demonstrate existing knowledge.
How to Create an Annotated Bibliography
- Selecting Sources
The first step is to select relevant and credible sources that pertain to your medical research topic. Look for peer-reviewed journals, books, and conference papers that provide valuable insights and data. Prioritize recent publications to ensure up-to-date information, unless historical perspectives are necessary.
- Citations
Each source should be cited according to a specific academic style (APA, MLA, Chicago, etc.). This citation includes all necessary details like author(s), publication year, title, and publication details.
- Writing Annotations
For each citation, write an annotation that includes:
- Summary: Briefly describe the main idea of the source.
- Evaluation: Critically evaluate the source for its reliability, validity, and bias. Discuss the author’s credentials and the publication’s reputation.
- Reflection: Reflect on how the source is useful for your research. Discuss how it contributes to your understanding of the topic or how it might shape your research methodology.
Writing an annotated bibliography can present various challenges, especially when dealing with extensive research. The sheer volume of sources to be analyzed and annotated demands significant time and effort, and each entry must be crafted according to precise academic standards. This meticulous task requires not only a deep understanding of the subject matter but also the ability to succinctly summarize and critically evaluate a wide array of information.
For students overwhelmed by the scope of their research or constrained by time, managing this task can be daunting. In such cases, seeking professional help can be a wise decision. Services like EduBirdie offer specialized assistance, allowing students to request write my annotated bibliography and receive expert help tailored to meet academic requirements and deadlines, ensuring a high-quality, comprehensive annotated bibliography that supports their research effectively.
Specifics of Creating an Annotated Bibliography in Student Medical Research
Creating an annotated bibliography in student medical research demands meticulous attention to detail and a deep understanding of the topic at hand. Each annotation must not only summarize the source but also evaluate its relevance and reliability in the context of medical research. Here are some specific considerations to keep in mind:
- Source Selection: Due to the rapidly evolving nature of medical science, it’s crucial to use the most current and peer-reviewed sources available. These sources should offer significant insight into the medical questions being studied.
- Clinical Relevance: Each source should be evaluated for its clinical relevance and potential impact on patient care, which is a central concern in medical research.
- Methodological Assessment: Pay special attention to the methodologies used in the research articles. A thorough understanding of these methods is essential to evaluate the credibility and applicability of the findings.
- Ethical Considerations: Medical research often involves critical ethical considerations, especially in human or animal studies. Annotations should reflect the ethical standards adhered to in the studies.
- Interdisciplinary Approach: Given the interdisciplinary nature of medical research, consider how each source interacts with others from different disciplines, such as biology, chemistry, or public health.
Incorporating these specifics into your annotations will not only improve the quality of your bibliography but also enhance your understanding of the complex and interdisciplinary landscape of medical research.
Tips for Effective Annotations
- Be Concise: Keep each annotation brief and to the point.
- Use Academic Language: Maintain a formal tone suitable for academic work.
- Be Critical: Analyze the strengths and weaknesses of each source.
- Reflect Personally: Make it clear how each source fits into your research context.
Examples of Annotations in Medical Research
Here’s an example of what an annotation might look like for a medical research paper:
APA Citation: Smith, J. (2020). Effects of New Alzheimer’s Medication. New York, NY: Health Press.
Annotation: This book provides a comprehensive overview of the latest developments in Alzheimer’s medication. Smith, a renowned neurologist, draws on numerous studies to discuss potential treatment breakthroughs. The book is well-researched, with extensive references to peer-reviewed articles. It is particularly useful for my research as it covers a gap in the literature regarding long-term medication effects. However, the book does not discuss alternative treatments extensively, which is a noted limitation.
An annotated bibliography is not just a formal requirement but a valuable component of academic research, especially in the medical field. It forces you to think critically about the literature, to assess its value to your own work, and to keep a clear record of the evolving landscape of medical research. By mastering this skill, you enhance your understanding of both the breadth and depth of your subject area, paving the way for a successful research project.
Revolutionizing Dentistry: The Latest Innovations in Dental Technology
Dentist appointments are usually so scary for a lot of people. They didn’t like the sound of the drill. Many of us hesitate to sit on the dentist’s chair. Because of this, many of us didn’t go to the dentist. But sometimes we really need it too. But things are getting better day by day. Dentistry is changing now. New inventions and cool technology are coming to assist us. These new things make dentist appointments easier. It’s also less scary. They also help the dentist do their job better. It means the people’s teeth get healthier. Let’s talk about some newest inventions. These technologies are making dentistry better for everyone.
Digital Dentistry
Digital dentistry means using latest technology to make dentistry easier and better. With this dentists won’t use messy stuff to make molds of your teeth. Now they can use digital tools to take accurate pictures of your teeth. This makes fillings or other procedures much more comfy. Now you don’t have to deal with gooey stuff in your mouth. It’s also called CAD/CAM. This is like magic for making artificial teeth. With this, dentists can quickly make new teeth. It perfectly fits in your mouth. This means you spend less time in the dentist’s chair. And also your new teeth look and feel better. Basically, this dentistry uses latest gadgets to make your dentist visits quicker. Also they are more accurate and less messy. So, you can smile big because your teeth are in good hands.
Laser Dentistry
Laser technology has made dentistry less scary. Now dentists won’t use drills and sharp tools. They can now use special lasers for lots of different treatments. These lasers are tiny. Moreover they are super accurate beams of light. They can do things like fixing cavities and shaping gums. They are also helpful for doing surgeries on soft tissues in your mouth. One of the best things about laser dentistry is that it’s not as painful as traditional methods. You feel less discomfort during the treatment. You can also recover faster. Plus, lasers are so precise. They can do their job without making your gums bleed much. With this you might not even need anesthesia. Lasers are so exact and gentler with your teeth. This means they can fix problems while keeping your natural tooth. This is great for your long-term oral health. If you’re scared of regular dentist tools, this is a good option for you. It’s a modern way to take care of your teeth. This technology keeps your smile shining bright.
Artificial Intelligence (AI) in Dentistry
This is the main innovation in the upcoming year. It’s a super smart assistant that helps your dentist make your teeth healthier. That’s what artificial intelligence does in dentistry. AI is like a really precise computer program. It can look at lots of information. Also it precisely takes pictures of teeth and has data about patients. It helps your dentist to figure out what’s best for your smile. Dentists use these special AI algorithms to study big sets of information about patient’s teeth. This helps dentists diagnose problems earlier. With this they can plan treatments that are right for each person. AI can help predict if someone might get a cavity soon. Also how braces might change their smile. With AI dentists can make smarter choices about your teeth. They can catch problems early. By this they can create treatments that are perfect for you. So in the future AI will help make dentist visits even better.
Conclusion
These cool new inventions are just the beginning of how dentistry is getting better and better. They make it easier for dentists to figure out what’s going on with your teeth. So they can do treatments more precisely. These innovations also make sure you’re comfy during your visit. It’s like stepping into an amazing future. Dentists are now able to give you even better care using these amazing new tools. With these they can even make a top-notch treatment to keep your teeth healthy.
If you want to experience these innovations in dentistry, BK Dental is here to serve! Their dental office is like stepping into the future. They have all the latest technology like digital dentistry and laser innovations for teeth. They can take super accurate pictures of your teeth without any mess. Their laser technology makes treatments easier and less painful. At BK Dental, they combine all these amazing technologies to give you the best care possible. Their goal is to make your smile the best.
In the future, dentistry will revive so many other innovations. It includes virtual reality (VR) and augmented reality (AR). With VR and AR you could take a visit inside your own mouth. Also can see what a treatment will be like before it even happens. How cool is that. So, the future of dentistry is full of new possibilities. We can’t wait to see what’s next!